
Shoulder Pain – Not A One-Size-Fits-All Approach
by Madison Warren, SPT
December 8, 2021
Photo by Otto Norin on Unsplash
"Shoulder Pain – Not A One-Size-Fits-All Approach" by Madison Warren, SPT
Do you have shoulder pain? No worries, you are not alone! Shoulder pain is reported as the third most common musculoskeletal condition seen by physicians and physical therapists. Although shoulder pain is slightly more common in women and associated complaints increase with age, shoulder pain can ultimately be due to many factors -strength, age, laxity, mobility, posture, occupation, comorbidities, stress, etc.
What is causing your shoulder pain? What can you do about this? Continue reading! The goal of this blog post is to inform you of the common types of non-traumatic shoulder pain and how physical therapists use evidence-based knowledge to treat shoulder pain based on signs and symptoms.
Are you lacking motion?
Mobility is determined by the ability of a joint to move through a range of motion. Mobility-based interventions are used to improve joint range of motion. For example, to raise your arm overhead to complete a tennis serve, the humerus must glide down on the scapula. Shoulder pain related to mobility deficits can come from the glenohumeral (shoulder) joint itself, as well as the cervical and thoracic spine.
Do you feel tightness in your neck and upper back?
Flexibility is determined by the length of a muscle that crosses a specific joint. To improve flexibility in a specific area, the surrounding muscles must be stretched. For example, to improve overhead motions or shoulder external rotation in swimmers, the pectoralis major and minor require stretching.
Do you feel “loosey-goosey” and like your shoulder slipping in and out?
Stability is determined by a group of small muscles working together to form a strong base from which our larger muscles can pull. Stability is related to muscle strength and power. Stability around a joint improves the overall strength of that joint and decreases the risk of injury. For example, for the scapula to rotate properly during shoulder movement, the rotator cuff muscles must provide stability.
So, which one do you need? Well, “it depends.” Some of us need mobility. Some of us need flexibility. Some of us need stability. Some of us need a combination of these for the shoulder to function properly and reduce pain. Physical therapists use clinical expertise and evidence-based practice to determine the appropriate exercises and techniques needed to treat a painful shoulder. Treatment is guided by the concordant sign that drives pain and disability. The concordant sign is defined as the pain, movement, or symptom causing dysfunction and functional deficits. Because everyone’s shoulder pain is different and due to different factors, diagnosis and treatment is not an “one-size-fits-all” approach.
Common Types of Non-Traumatic Shoulder Pain:
Subacromial Pain Syndrome:
Subacromial Pain Syndrome, also known as Subacromial Impingement, is defined as pinching of the supraspinatus and/or the subacromial bursa under the acromion. Impingement is associated with microtrauma, microtrauma, or functional instability. Most non-traumatic shoulder impingement pain is associated with muscle imbalances in those that work to stabilize the scapula. This results in reduced scapular control and overuse of the rotator cuff muscles. Other common causes include faulty joint mechanics, muscle shortening, rotator cuff degeneration, reduced motor control in the glenohumeral or scapular stabilizers, poor posture, adhesions, or increasing age. Subacromial Pain Syndrome is common in overhead athletes or those who perform repetitive overhead motions, leading to pain along the anterior-lateral shoulder near the deltoid insertion. Patients with Subacromial Pain Syndrome will report pain with overhead motions, specifically between 60-120 degrees of shoulder elevation. The prognosis worsens when pain lasts more than three months. Treatment focuses on what is causing the narrowing. In some, the narrowing is due to muscle weakness and poor stability. In some, the narrowing is due to poor posture and reduced flexibility. In some, the joint does not move properly and needs mobility. Some of you may need all three of these.
Tendinopathy:
Tendinopathy can progress from Impingement. A reduction in the subacromial space causes tendon irritation and degeneration. Degeneration causes tendonitis and can progress to degenerative tendinosis, a partial thickness tear, and eventually a full-thickness tear of one of the rotator cuff muscles. Tendinopathy can occur in the Long Head of the Biceps tendon or one of the 4 rotator cuff muscles (SITS: Supraspinatus, Infraspinatus, Teres Minor, Subscapularis). The causes of tendinopathy are similar to those of Impingement. If detected in the early stages (tendinosis), the pain will cease with rest. Treatment is focused on strengthening the surrounding weak muscles to provide stability, improving flexibility and mobility, and addressing proper positioning.
Glenohumeral Instability:
Glenohumeral Joint Instability is a loss of dynamic control, concavity compression, or motor control in the shoulder joint. The glenohumeral joint is a ball-and-socket joint designed for mobility, but too much mobility can be detrimental. Glenohumeral Joint Instability occurs most often due to trauma, repetitive overuse, ligament laxity, or reduced motor control in the rotator cuff muscles or scapular stabilizers.
One example of glenohumeral joint instability is a labral tear. Repetitive overhead activity can lead to fraying of the labrum in the shoulder joint. A labral tear lessens the compressive forces that hold the humeral head in the glenoid socket. Labral tears are commonly seen in those who perform repetitive overhead activities, causing progressive fraying. If the tear is severe, it is not uncommon to see a partial-thickness tear of the Supraspinatus muscle.
Another example of glenohumeral instability is general instability and laxity in the shoulder. General instability can be due to a lack of muscular control and overall muscle weakness. Here is an example. Meet our patient…. Me, a third-year DPT student with functional instability in both of my shoulder joints.
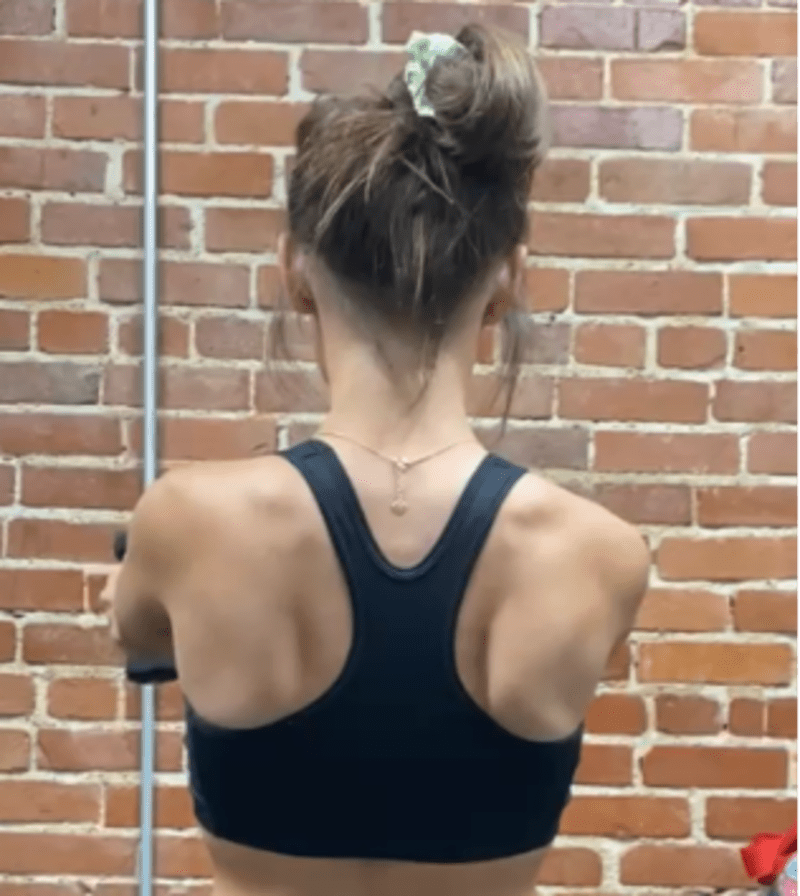
Bilateral Scapular Winging
I am a former college tennis player and cheerleader, so I have repeatedly been moving overhead all my life. Is that the only cause? Sadly, no. My posture is definitely not ideal. I sit in front of a computer studying much of my day and have allowed my body to just slump over. This has caused my muscles to become tight. I am also weak in the shoulder and scapular stabilizing muscles (refer to the picture above). I have bilateral scapular winging due to lower trapezius and serratus anterior weakness. Needless to say, I need to practice what I preach and do something about my instability.
Patients with Glenohumeral Instability usually complain of feelings of the shoulder “slipping in and out,” a loss of velocity when throwing, or clicking and catching in the shoulder joint. Pain is usually intermittent and is associated with overhead movements or specific motions. Treatment for shoulder instability should address many areas, depending on the patient: normalize scapulohumeral rhythm, normalize arthrokinematics in the joint, balance the ligament structures, and normalize the function of the rotator cuff muscles, biceps, and scapular stabilizers.
Adhesive Capsulitis:
Adhesive Capsulitis is formerly known as Frozen Shoulder and occurs when the shoulder capsule becomes thick and adheres to the humeral head. The onset of Adhesive Capsulitis is slow, and the primary cause of Adhesive Capsulitis is idiopathic. The secondary cause is due to immobility following trauma or surgery. For example, if a patient injures the shoulder, elbow, wrist, or hand and avoids moving the entire extremity for prolonged periods, adhesions can form and cause stiffness in the joint. Risk factors for Adhesive Capsulitis include diabetes, hypothyroidism, lower BMI, and family history. Patients usually complain of constant, nagging pain at the deltoid insertion. Pain occurs at night, and patients are unable to sleep on the affected side. Shoulder abduction, internal rotation, and external rotation active range of motion are most often limited. Passive range of motion and humeral head joint mobilizations are commonly limited in all directions. Treatment is based on irritability levels and symptoms. Generally, mobility is the main key to treating Frozen Shoulder. As symptoms improve, stability and flexibility interventions will be added to the plan of care to prepare patients for return to functional activities.
Do you feel like you are dealing with any of these things? Do you need mobility interventions to improve joint range of motion? Do you need flexibility interventions to improve muscle length and ultimately improve range of motion? Do you need stability interventions to improve the strength of joint stabilizing muscles and reduce the risk of injury? Do you need a combination of these things (like me) to reduce your shoulder pain? Remember, treatment for shoulder pain is not the same for everyone - it is not a one-size-fits-all approach. Physical therapists can help you determine the underlying cause of your shoulder pain and what exactly you need to conquer this. Contact Physiolete Therapy and Performance today and let us help you tackle your shoulder pain!
References:
MBC - https://orthoinfo.aaos.org/en/diseases--conditions/shoulder-pain-and-common-shoulder-problems/

