NEUROPLASTICITY: USE IT OR LOSE IT
by Skylar Metzel, SPT
April 7, 2021
Photo by Jesse Martini on Unsplash
NEUROPLASTICITY: USE IT OR LOSE IT by Skylar Metzel, SPT
Are you familiar with the saying “Use it or lose it”? We tend to hear this saying in regard to our strength, flexibility, endurance, or skill level in regard to a specific sport or activity. This same saying also applies to our brain functions. Our brain controls the initiation, coordination, fluidity, speed, accuracy, and precision of every movement we make. So, what happens when we neglect the areas of our brains that control these activities? We lose our ability to perform these functions at normal or even expert levels.
In order to help you wrap your “brain” around what we are about to get into, we are going to use a parable to help illustrate our lesson on neuroplasticity.
Meet Craig. Craig is a pitcher for the Tuscaloosa Yellow Hammers, a minor league baseball team that doesn’t actually exist. Craig injured his left ankle sliding into home during yesterday’s doubleheader. He visits his team doctor the next day who tells him that he has a left ankle fracture. Craig will need to wear a boot and he will be non-weight bearing and on crutches for several weeks. Craig goes to see his physical therapist after his appointment with his doctor and is devastated about what his injury might mean for his baseball career.
Let’s get back to our lesson on neuroplasticity. Neurons are the basic working unit of the brain. Neurons have the ability to change themselves, this is neuroplasticity. (1) Let’s break this down; neuro=neuron and plastic=moldable. Neurons can change in a positive manner by reinforcing normal and skilled movement functions. However, they can also change in a negative manner by reinforcing abnormal movement functions. Even worse, neurons that aren’t engaged can lose the ability to assist us in performing certain functional movements altogether. What is amazing is that we have the ability to make movement function changes and alter our brains through neuroplasticity within a matter of seconds.(2) An easy example of this would be providing a mirror and a verbal cue for someone who has unknowingly squatted knees inward for years. By providing a mirror and giving them a simple cue to keep their knees straight, you are training their brain to create new and normal movement patterns. It is kind of like doing brain surgery without any sort of surgical intervention.
Within our brain, we have maps for each body part located in the sensory and motor cortex. These maps are represented in what is we call the “homunculus.” In the picture of the homunculus below, we can see that different body parts are represented by different-sized maps.
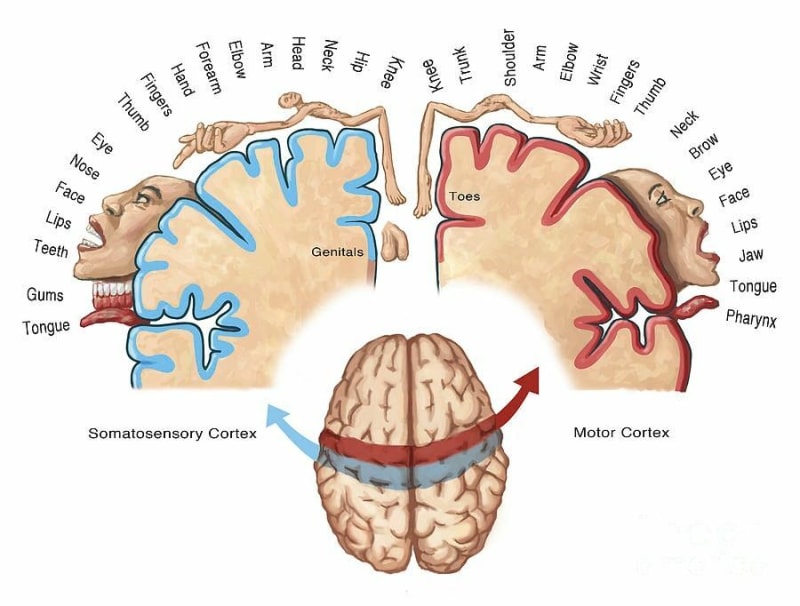
Our hands have a much bigger map because they are body parts that we use to feel and sense the most. We also perform fine and detailed motor movements with our hands so those maps need to be larger. In contrast, our ankles have a much smaller map than our hands on the homunculus. This is because our ankles are involved in large and gross motor movements, like walking. We also don’t normally use our ankles to perform fine motor movements. As a body part is used repetitively for a certain function, the respective map for that body part becomes sharp and crisp. If we don’t use a specific body part due to pain, surgery, or an injury, that specific map for that body part can become smaller or get “smudged”(2). This “smudging” can cause us to develop chronic pain because our brain is perceiving sensations abnormally (2,3). “Smudging” can also create abnormal movements and reduce our ability to perform specific activities or tasks at a high functioning level.
Let’s say Craig decided to skip physical therapy after his left ankle injury because he didn’t think it was important. He stayed in the boot until his doctor cleared him based on his fracture being healed on X-ray, but he tried to jump back into baseball without any proper rehabilitation. He never did any range of motion or strength exercises and no one ever corrected the limp he had after getting out of the boot. The ankle map on his homunculus started to “smudge” and become less crisp and clear. Now he is having some generalized lower leg pain, he can’t perform any fine motor movements with his toes (important for balance), he has abnormal gross motor movements of his ankle, and his sensation is altered in his entire left lower leg. Years later he continues to have these symptoms in his left leg and ankle from negative neuroplastic changes. You may be asking yourself, could some of this have been prevented? Absolutely.
Below we are going to discuss how we can keep the maps of our brain engaged, crisp, and sharp so that we can stay functioning at normal and high levels with regards to activities of daily living and other movement skills. After a surgery or injury, you may experience limited weight-bearing precautions, you may have range of motion limitations, and you may have precautions with regards to what you can/can’t do with the surgical or injured area (3). While these limitations may allow a certain area of your body to heal initially, they may also cause you to develop a fear of movement or chronic pain and dysfunction down the road if certain impairments aren’t addressed in a safe and timely manner. How can you improve neuroplasticity in a positive manner after surgery, an acute injury, or even with chronic pain? See below!
Graded motor imagery (GMI) is composed of 3 stages that challenge and strengthen the brain to improve neuroplasticity positively. There are 3 stages: laterality, imagery, and mirror therapy (2,4). It is important to note that each stage is not mutually exclusive, nor does each stage have to occur to make a full recovery. You have the flexibility to jump from one stage to another, back to a stage, or skip a stage.
Stage 1 - Laterality (2,4)
- Laterality is having the ability to decipher between a left and right body part. Seems kind of silly right? Looking at an image and not being able to tell whether it is a left or right body part? With long-lasting or chronic pain, smudging on the homunculus can actually affect your ability to decipher your left from your right, depending on what part of your body is injured.
- An example of laterality: While Craig was non-weight bearing in his boot his physical therapist had him perform exercises to improve laterality. At the end of physical therapy when he was elevating and icing his ankle after his session, his physical therapist had him circle all the left ankles in the latest issue of Sports Illustrated. Craig thought this sounded a little crazy at first, but he soon realized how hard it actually was. He did this after each session and started to notice that it got easier and he got faster. Little did Craig know, he was sharpening the map in his brain that covered his left ankle on his homunculus.
- Fun fact, there are actually flashcards and software apps for lateralization therapy. The pictures below depict what the flashcards look like and can be individualized to a person’s unique injuries. Left hand or right hand? Left foot or right foot? You make the call!

photo from - http://www.gradedmotorimagery.com/
Stage 2 - Imagery (2,4)
- Imagery is a stage many of us are familiar with. I was a cheerleader back in high school and prior to any routine, my team would sit in a circle with our eyes closed and imagine ourselves going through a full-out routine. We would picture ourselves doing each stunt or tumbling pass perfectly. This is imagery. It is imagining yourself completing a task, even as simple as bending your knee throughout your full range of motion without pain. This stage preps the brain before the body, and it can help reduce the anxiety of returning to a specific movement or sport.
- An example of imagery: While Craig was performing his ankle range of motion exercises he told his physical therapist that he was bored and wished he could be pitching instead of drawing the alphabet with his ankle. His physical therapist told him to imagine himself pitching, every single phase of his pitch from start to finish between sets of his exercises. Craig didn’t realize it at the time, but he was creating strong and sharp maps in his brain that would later improve his performance and reduce his risk of developing fear avoidance behaviors.
Stage 3 - Mirror Therapy (2,4)
- Mirror therapy is a stage that utilizes a mirror to reflect the non-surgical or non-injured body part. The mirror image of the unaffected side creates an illusion that the involved limb is moving within a normal range, with normal function, and without pain or symptoms. Essentially, we are tricking the brain and sharpening the maps of the specific body part on the homunculus of the injured area. Mirror therapy is an exercise that is often used in patients after an amputation who are experiencing “phantom pain” in the limb that has been amputated. The mirror can instantly take away phantom pain by the mechanism we have described above, pretty cool right? The mechanism is similar for someone experiencing chronic pain.
- An example of mirror therapy: Craig asked his physical therapist why he was still having ankle pain pointing his foot downward weeks after he was out of the boot. “The bone is healed, I don’t understand why I am still having pain in this area?” His physical therapist initiated mirror therapy and immediately he reported a reduction in ankle pain. “How weird, when I watch my right ankle in the mirror it reduces the pain in my left ankle!” Again, Craig didn’t realize that each stage of GMI therapy would help him reach his long-term goals.

How often should you perform these GMI exercises? For people who are candidates for GMI it is recommended that you perform these exercises for 2 hours per day, every day, for 2 weeks. (2) Now that isn’t always the case, the length will depend on your ability to regain sharpness of the maps in your brain and how quickly your symptoms are improving.
Good news, Craig didn’t skip his physical therapy appointments. He completed a successful round of physical therapy after fracturing his ankle which included GMI therapy, range of motion exercises, functional strength training, proprioception training, and return to sport exercises. He joined the Tuscaloosa Yellow Hammer’s for the next season and ended up having the fastest pitch in the minor leagues. He had no issues with his ankle and he felt it was even stronger on the pitching mound, probably some of the extra balance and proprioception training he did in physical therapy (a story for another day).
In summary:
- Brains are neuroplastic meaning they can change in a positive manner or a negative manner depending on what we do (or don’t do).
- Our brain is the command center for all things that we do. We need to make sure we are training it, keeping it sharp, and engaging it every day (2).
- The brain, specifically the sensory and motor cortex, is filled with maps for each body part. When the body part is used frequently and correctly, the map remains sharp. When a body part is not used frequently, that map may become smaller or smudged. If a body part is not used, the map disappears.
- After an injury or surgery, it is very important to regain range of motion, progress weight bearing to tolerance safely, improve strength, and decrease pain. It is critical that we engage our brains during this time as it too has control over achieving a full recovery.
- Utilizing the Graded Motor Imagery (GMI) method is beneficial in keeping the brain active and stimulated, however, returning to sport and activities is a multi-modal and multi-system approach (3,5). This type of treatment is not the end-all be-all and should be utilized in conjunction with motor control exercises and a graded exposure to return to normal activity or sport.
If you have further questions, are experiencing pain, or would like some clarification on any of the information you read today, reach out to us at Physiolete Therapy and Performance. You can call us at 205-409-8060 or email us at [email protected]. We provide complimentary screenings and would love to assist you in any way we can.
References:
- Larsen DS. Why neuroplasticity? Journal of Neurologic Physical Therapy. 2012; 36(2): 110-111. doi:10.1097/NPT.0b013e3182567076
- Louw A. The brain, athletes, and sports performance. Medbridge.
- Baller EB, Ross DA. Your system has been hijacked: the neurobiology of chronic pain. Biological Psychiatry. 2017;82(8). doi:10.1016/j.biopsych.2017.08.009
- Complete guide to graded motor imagery (GMI) for CRPS. Burning Nights CRPS. https://www.burningnightscrps.org/graded-motor-imagery-gmi-crps/. Published 2021. Accessed April 7, 2021.
- Motor control and learning. Physiopedia. https://www.physio-pedia.com/Motor_Control_and_Learning. Published 2021. Accessed April 7, 2021.

